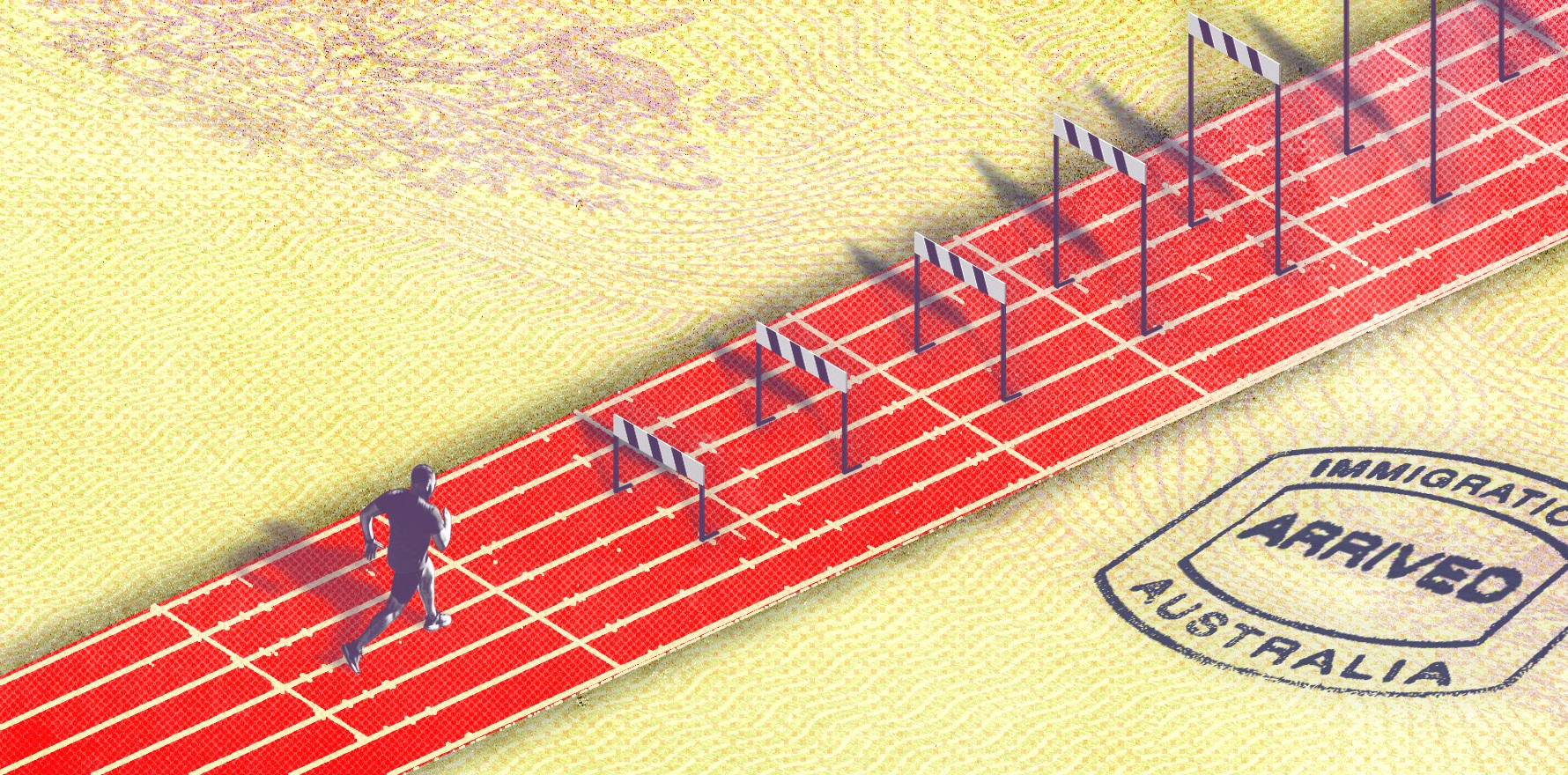
The Australian and New Zealand College of Anaesthetists is the latest medical organisation to question the value of the incoming registration fast track for overseas trained doctors.
AHPRA’s new, fast-tracked registration pathway for specialist overseas trained doctors is meant to process its first GPs this month – but so far, there’s been radio silence from the regulator.
It has led the Australian and New Zealand College of Anaesthetists (ANZCA) to believe that the system will not be ready to process its first anaesthetists, psychiatrists, obstetricians and gynaecologists by the end of December.
The controversial new initiative took the medical colleges by surprise when it was first announced in April this year.
Effectively, it will allow overseas trained doctors who have completed specialty fellowship in countries with substantially similar programs to bypass medical colleges and go straight to the board to obtain Australian registration.
Successful applicants will only have to undertake six months of supervised practice, cultural safety education and an orientation to the Australian healthcare system.
Adding fuel to the fire was a tight turnaround set by state, territory and federal health ministers, which meant a shorter-than-usual consultation period.
While the AHPRA site still lists “late October 2024” as the launch date for the GP pathway, it still has not published the list of qualifications that are eligible under the scheme.
An AHPRA spokesman told Allergy & Respiratory Republic today that it was still on track to launch in October and that “more detail is coming soon”.
It also confirmed that qualifications from the United Kingdom, New Zealand and Ireland would be on the list.
“The impression we have is that there’s still a lot of things to be sorted out at the AHPRA end, and that in fact, they’re finding it harder [to implement] than they expected,” ANZCA president Professor Dave Story told ARR.
“I think it is unlikely that they [will make their planned implementation date], but they are under ministerial pressure and one of our concerns is they may rush it.”
ANZCA has called for a pause on the rollout of the pathway until more information is provided.
“We see this principally as a patient safety problem, because the nature … of anaesthesia is that an error of judgment or an error in procedure can harm or even kill a patient very quickly, or lead to long term disability,” he said.
While the list of eligible qualifications is yet to be confirmed, Professor Story said he was relatively confident that training programs in the United Kingdom and Ireland would be included.
“They are substantially comparable [training courses], but not completely,” he said.
“There are two components to that, and one is some of the cultural differences – they’re both more hierarchical societies.
“And one of the things we like all our trainees to do – and we don’t know whether AHPRA will require this or not – is a course on effective management of anaesthesia crises and one of the things for the SIMGs is to try and instil in them the nature of Australian interactions in a crisis, which may be much more egalitarian than in England and Ireland.”
Related
Professor Story was similarly unimpressed with AHPRA’s proposal for six months of supervised practice.
“One of the major components of our assessment of comparable SIMGs is a practice component, so they have at least six months of supervised practice – but also from our perspective, it’s mentored practice,” he said.
“Towards the end of that is a workplace-based assessment which includes review of cases, and that’s one of the bits that will not be in the AHPRA pathway, which we think is really concerning.”
If the end product is a doctor who will be allowed to practice completely independently within Australia, Professor Story said, there is good reason to have an abundance of caution.