Prescribing ‘just in case’ antibiotics is not without risk.
Professor John Turnidge AO and Associate Professor Liz Marles from the Australian Commission on Safety and Quality in Health Care (the Commission) explain the latest trends in antimicrobial use and resistance from the AURA 2023 report.
Since the First Australian report on antimicrobial use and resistance in human health was released in 2016, the Commission has closely monitored trends over time to inform what actions are needed in our health system to prevent the rise of antimicrobial resistance (AMR).
Knowing how we are faring against a baseline is useful as we respond to the threat of AMR.
The AURA reports analyse data from the Antimicrobial Use and Resistance in Australia Surveillance System (AURA), which captures the magnitude, distribution and impact of AMR, and identifies emerging issues and trends.
It is not widely known that Australia has one of the highest antimicrobial community prescribing rates in the world, in contrast to countries with comparable healthcare systems and disease profiles such as England, Canada and the Netherlands – although we have been working for some years to turn this around.
It was therefore gratifying to see a downward shift in patterns of community antimicrobial use during the pandemic in the Fifth Australian report on antimicrobial use and resistance in human health (AURA 2023), published this month.
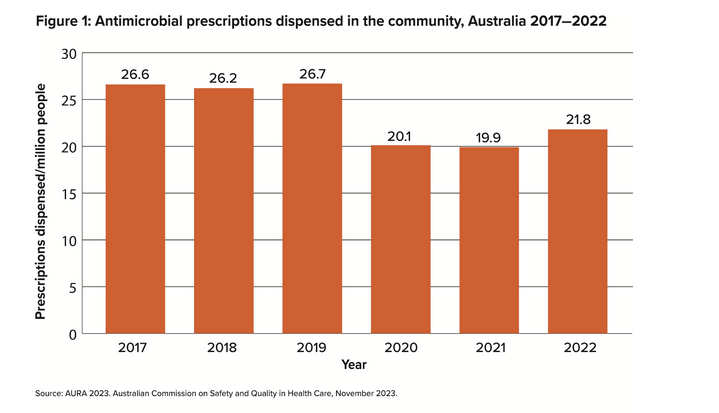
While not the lever we would have chosen, the covid pandemic had a major impact on antimicrobial use in Australia. It was driven in large part by change in social interaction and behaviour, with a dramatic 25% reduction in antimicrobial use during the two years from 2019–2021 (refer to Figure 1).
There are many potential reasons for this decline, including social distancing during the pandemic, which resulted in fewer people getting respiratory viral infections and seeking treatment. That in itself reflects just how often antimicrobials have been prescribed historically in Australia for respiratory viral infections.
While we saw a rebound in antimicrobial use in the community last year – up by nearly 10% from 2021 to 2022 – it was still 18% lower than in 2019, which is well below pre-pandemic levels. There is hope that this will be sustained in the coming years.
And Australia has a long way to go to compare with other countries such as the Netherlands.
As healthcare practitioners and prescribers, we face a clear opportunity to sustain improvements in antimicrobial prescribing. Success is partly in our hands – it relies on appropriate prescribing and how we communicate with patients to influence their use.
AMR is reducing the effectiveness of some of our most important medicine resources. Not using antibiotics unless they are warranted and using them according to guidelines is vital, as is reinforcing messages to patients that many infections get better without antibiotics.
National outlook for antimicrobial use
In the community, the principal sources of Australian prescribing data are the Pharmaceutical Benefits Scheme (PBS) and the Repatriation Pharmaceutical Benefits Scheme (RPBS). Other prescriptions that are not included in these data are dispensed privately.
It is encouraging that we have upheld an overall decrease in antimicrobial use in the community over the past few years.
In 2022, 21.8 million antimicrobial prescriptions were dispensed, up 9.6% from 2021 (19.9 million), although this was still well below the use prior to the covid pandemic.
In 2022, 36.6% of the Australian population (9.5 million people) had at least one antimicrobial supplied under the PBS or RPBS. This is slightly higher than in 2021 when the figure was 32.9% (almost 8.5 million people). More information on analyses of these data and local data at the SA3 level is available on the Commission’s website.
MedicineInsight is the large general practice dataset which collects longitudinal de-identified clinical data from participating general practices across Australia. MedicineInsight helps us to understand appropriateness of antimicrobial prescribing in the community.
In MedicineInsight contributor practices, antibiotics were prescribed for approximately 80% of acute bronchitis cases in the community for patients aged 18–75 years in 2020 and 2021. Antimicrobials are not recommended for the management of acute bronchitis.
As understanding about AMR builds in the community, we need to continue to have robust conversations to counter patient requests for antibiotics when they are not appropriate, and which won’t help them get better if they have a cold, flu or other viral infection.
The Commission’s patient information sheet ‘Do I really need antibiotics?’ can help doctors navigate these discussions. Most importantly, we need to explain to patients that antimicrobials are not free of side effects, so taking them ‘just in case’ is risky. Clostridioides difficile infection (CDI) is one such troublesome side effect and is on the rise in the community.
When antibiotics are necessary, it is important to ensure the patient understands why they are taking the antibiotic and the duration of therapy. Clear documentation of the expected duration of therapy for antibiotics minimises confusion and ensures the individual has the appropriate course of therapy.
Rise in community-onset CDI
A compelling finding in the AURA 2023 report is the increase in the rate of community-onset CDI from 2020 to 2021.
There is a perception that CDI is only an issue for patients in hospitals – but the AURA 2023 report shows that more than 80% have been acquired in the community.
CDI is a known adverse effect of antimicrobial use, which all prescribers can help control by avoiding antibiotic overprescribing.
Rising incidence of CDI occurring in the community highlights how important it is to be aware of this condition at a community level, and not just at the hospital level.
STIs back on the radar
It is unsurprising that physical distancing and travel restrictions imposed as public health measures in response to the covid pandemic had an impact on many communicable diseases in Australia, including sexually transmitted infections (STIs).
Since restrictions have eased and international travel increased, cases of highly resistant gonorrhoea and multidrug-resistant Shigella are also rising.
In 2021, Neisseria gonorrhoeae that has reduced susceptibility to ceftriaxone increased 37-fold, an ominous development, while multidrug-resistant Shigella species more than doubled.
Remembering to ask about a patient’s recent travel history is important for doctors, as it may have dropped off the radar during the pandemic.
With rising AMR in STIs, particularly for men who have sex with men, reinforcing public health messaging is especially important. State and territory prevention and control programs and outbreak response strategies are also important for these infections.
Judicious use of antimicrobials
The AURA 2023 report is a reminder that judicious use of antimicrobials is more important than ever because of resistance – particularly as people present more frequently with respiratory infections as the pandemic eases. AMR doesn’t only pose a collective risk in the community; it also drives risk of harm to individuals.
In more serious cases, we may be left with no antibiotic options for some patients due to resistance, especially when combined with medication allergies. Other individual risks are the impact on the microbiome and emerging evidence that antimicrobial use may contribute to long-term chronic illness later in life.
Elsewhere in the community, AURA 2023 highlights concern about the use of antimicrobials in aged care homes. It is important to follow antimicrobial stewardship guidelines that are appropriate to the aged care setting. Resources developed by the Commission summarise AURA 2023 highlights and priorities for action by healthcare workers in a range of settings, including aged care and primary care.
This week is World AMR Awareness Week (WAAW). As we progress to the post-pandemic years, there’s no better time to take stock and consider the role of general practitioners as prescribers and stewards of antimicrobials.
This article was developed with Kristin Xenos from the Commission’s AURA team.
Visit safetyandquality.gov.au/aura2023
Professor John Turnidge AO is Senior Medical Advisor for the Commission and an infectious diseases physician and microbiologist. He has led national surveillance for antimicrobial resistance and usage in human health since 2014.
Associate Professor Liz Marles is a Clinical Director for the Commission and a general practitioner. She is currently Chair of Therapeutic Guidelines, past President of the Royal Australian College of General Practitioners (RACGP) and a member of the RACGP Council.


