The Australian study found several bacterial species correlated with reduced lung function.
Patients with chronic obstructive pulmonary disease have a distinctly different gut microbiome from their healthy peers, according to Australian research published in Nature Communications.
It is the first study of the gut microbiome in COPD patients, and suggests faecal sampling may be a way to monitor the deadly disease.
Director of the Centenary UTS Centre for Inflammation Professor Phil Hansbro said that at a conference in 2012, a presenter had mentioned that people with COPD were roughly three times more likely to get Crohn’s disease, and around half of people with Crohn’s have pulmonary inflammation.
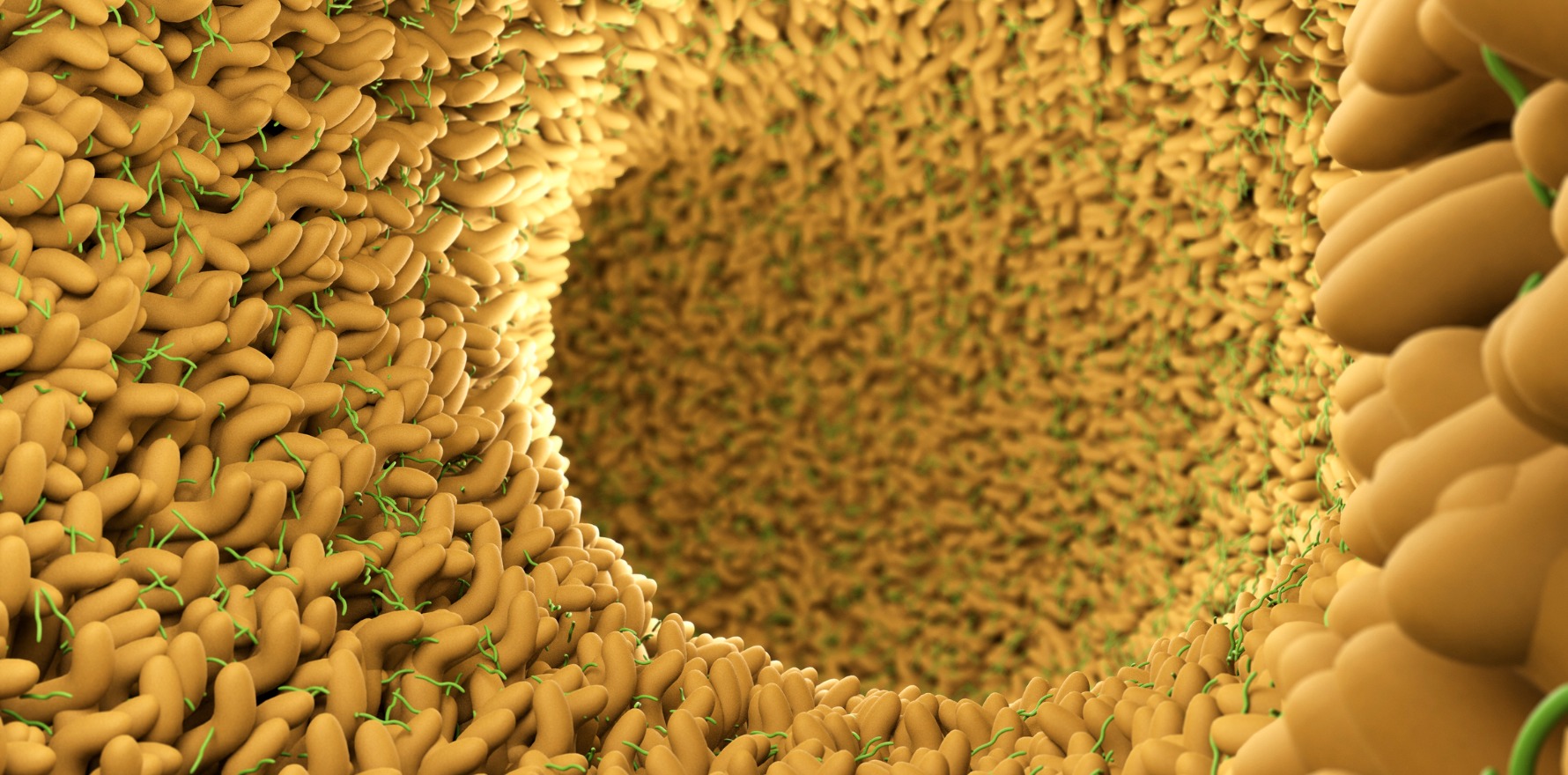
“A big part of the gut is its huge microbiome, and microbiomes produce metabolites,” senior author Professor Hansbro said.
“I got to thinking: was this a connection between the gut and the lung – the gut-lung axis?”
Professor Hansbro and colleagues collected faecal samples from 28 COPD patients and 29 healthy controls along with information on their diet, smoking status, and medication history.
They looked at which bacteria were in each sample and in what proportions. They also analysed the metabolome, including the genes expressed and waste by-products of the bacteria.
The team found 146 bacterial species differing between the two groups.
But several species, including Streptococcus sp000187445, Streptococcus vestibularis and multiple members of the family Lachnospiraceae correlated with reduced lung function.
“The crux of the study is that we can match changes in the microbiome with changes in the genes that they produce, with changes in metabolites circulating in people, which are correlated with disease in COPD patients,” Professor Hansbro said.
Finding lots of streptococci in the faeces samples was a “big surprise”, he added.
“Streptococci are primarily respiratory bacteria so finding these in the gut provides further evidence of gut-lung cross-talk. This was obviously a gut study, but I think we would find gut bacteria in the respiratory tract as well.”
Transfer of streptococci from the oral microbiome might be one explanation, via increased microaspiration of the airways with pharyngeal secretions in COPD patients, the authors wrote.
They found no difference in microbiome composition between current smokers compared to non-smokers with COPD. This suggests the differences between the COPD and control group were not being driven by the influence of cigarette smoke on the gut microbiome, they said.
“Interestingly, we observed a lower dietary fibre intake in participants with COPD compared to controls based on dietary surveys, which may contribute to both differences in gut microbiome profile and COPD pathology,” the authors wrote.
“Some soluble fibres act as prebiotics, providing a selective growth substrate, leading to changes in bacterial number and diversity and increased production of immunosuppressive by-products, which have been shown to reduce airway inflammation in both animal and human models of asthma.”
One limitation of the study was the “medium-sized” cohort, Professor Hansbro said.
“We’ve also not shown cause and effect with this study, which is why we are currently doing mechanistic studies in animal models of COPD to demonstrate this.”
The findings pointed to possible new treatment approaches, he said.
“Can we modify the microbiome with, say, microbiome transfers, or changes in diet that will cause the outgrowth of different species of bacteria? We might be able to identify beneficial bacteria and use those as treatments.”
Future studies might look at variations in the microbiome and metabolome over time since this study looked at one time-point only.
“We might also ask how these microbiomes are altered by the different treatments that people take, and if there are differences between people who frequently exacerbate versus relatively stable people.”