High stress, high stakes environments are rife with conflict.
It was not a face I was expecting to see.
I recently crossed paths at a conference with a long distant clinical supervisor from my years as a junior doctor. My recollection was that it had not been a relationship that was supportive nor encouraged me to reach my potential.
There had been occasions over the years that with the knowledge and wisdom of a senior clinician, I had rehearsed the eloquent but scathing feedback I wished to deliver. I wanted to share the distress that her leadership had caused during my formative years.
On this occasion, though, the carefully rehearsed words never passed my lips. Given I had just presented a plenary on conflict resolution in the workplace, I felt it was disingenuous to pull the pin on that particular grenade.
The chance meeting caused me to reflect on that era of my career and wonder whether had I possessed my current knowledge of the means to resolve conflict, my experience would have been more positive.
Hospitals are rife with conflict.
Why? Because they are high stress, high stakes environments.
It’s so interesting how some things never seem to change. In 2002, Drs Marco and Smith published a perspective on conflict in the emergency department. They suggested that emergency departments are a potential melting pot of conflict, given differences of opinions and value systems, fatigue and unrealistic expectations from both clinicians and patients. I am an emergency physician, so that’s my everyday world.
When conflict is handled poorly, it has the potential to divide the team and can impact negatively on patient care. Equally as important, it erodes the satisfaction of staff which can lead to burnout and mental health issues. Frequent destructive conflict can cause morale and staff retention to plummet. Conflicted departments see more complaints and medical errors and clinical directors are acutely aware how much valuable administration time this consumes. More importantly, the patients suffer higher morbidity and mortality rates.
What does workplace conflict look like?
Conflict often resembles rudeness, incivility and a lack of respect. It can be overt or it can be subtle. It can be expressed verbally, through the words we use, or through sarcasm and tone. It can be expressed non-verbally through eye-rolling, defensive posturing and body language.
What is the evidence that workplace conflict is harmful?
Research has shown that when clinical staff are exposed to rudeness in the workplace, there is a reduction in both the quality of communication and diagnostic accuracy.
Civility Saves Lives is a group of health care professionals in the UK aiming to raise awareness of the power of civility in medicine. When someone is rude to us, just mild to moderate rudeness, clipped tones, eye rolls, not even yelling or shouting, our bandwidth is reduced, and we carry it with us through the day. Bandwidth is our mental capacity at any one time so rudeness must affect our ability to care for patients.
What about if clinicians just witness the rudeness? It’s contagious! We know that the way someone was just treated is how they are likely to treat the next person they encounter.
In fact, in a study including 6000 nurses and nearly 40,000 patients in Hamburg looked at whether the nurses’ experience of their workplace culture impacted on their interactions with their patients and subsequently on their patients’ experiences.
Can you guess what they found?
Indeed, they found that staff who experienced a positive civility climate were more likely to pay forward the relationship experience and display civility to their patients. This in turn improved patient experience outcomes.
Schrepel and friends researched how professional identity and loyalty to one’s own team primes the hospital setting for conflict. The looked particularly at emergency and internal medicine relationships because transitions of care are important for maintaining patient safety.
Conversations regarding admission represented the majority of interactions between these two specialties. While differences of opinions in these conversations can lead to new differential diagnosis and treatment plans, when disagreements dissolve into interpersonal conflict, the outcome if often harmful. The object of the study was to look at the social interactions during these conversations that contribute to moments of conflict.
They interviewed clinicians from both specialties and found that each specialty acted to protect their own and thought their own style of clinical care was superior. Forcing or defending an admission was seen as an attempt to gain control in the battlefield that is healthcare. Being succinct and direct regarding the need for admission is an emergency doctor’s attempt at efficiency, however inpatient colleagues may feel disempowered by such assertive language.
When the researchers saw the formation of teams within teams, inclusive of each specialty and clinicians acting with humility and acknowledging uncertainty, the power struggles dissolved. Their conclusions were that multidisciplinary teams and actions to improve social capital promoted trust and mitigated conflict during ED consultations.
Our Canadian colleagues also explored the causes of and protective factors for conflict during ED consultations. To the surprise of no one, they found that dealing with a person with a poor reputation with poor communication skills was more likely to precipitate conflict. Those running with a personal agenda and providing inappropriate care were also prone to conflict. Conversely, a clinician with a collaborative reputation, with whom prior good experience had been had, who expressed empathy and met expectations of care protected against conflict.
Simulating civility
Health care professionals are increasingly turning to simulation to develop clinical skills and acumen. It should come as no surprise that simulation is being used to train health professionals in the skills of conflict resolution.
These Spanish colleagues published a literature review that outlined the success of a variety of programs using role play, reflective practice and audio-visual aids to train clinicians in the skills of mediation, communication and emotional intelligence. The skills were able to be translated into clinical practice and they saw a reduction in errors. Of course, almost every paper suggested that more research was required.
So how can we do better?
To start, we can turn up to work with the intention that we will be kind & compassionate, to patients and colleagues alike. Most people don’t arrive with the intention of being rude and to seek out conflict, however it occurs when we get busy, hungry, angry, tired and overworked. Sometimes our best intentions are not enough.
We need to create better systems in our workplaces to minimise the opportunity for conflict. Initiatives such as agreed admission pathways and care bundles for specific conditions to enable seamless transitions into hospital. Structured referral tools like SBAR make it easier to speak the same language and provide the essential information to those around us.
As an individual, we need to learn effective communication techniques and conflict resolution skills. Yes, these are skills that can be taught. And as senior staff, we need to role model effective conflict resolution skills to all the staff on our team.
This brings us back to our friends, Marco and Smith
Drs Marco and Smith developed a model on constructive ways to manage conflict, specifically in the ED, though in truth, these tips are good rules for life.

Throwing the gauntlet
My challenge to you is to change the way you think about conflict.
Change your frame to see conflict in the workplace as an opportunity, not a threat or something to be avoided at all costs.
Conflict handled respectfully, can be a wonderful opportunity to build positive relationships & gain the respect of your colleagues. It can also be an opportunity to solve problems and to improve the way you work together as a team.
Don’t shy away from it, when you see it happening, I encourage you to run towards it and try to demonstrate effective, mature conflict resolution strategies for your junior staff.
This is how we change the culture, one interaction at a time.
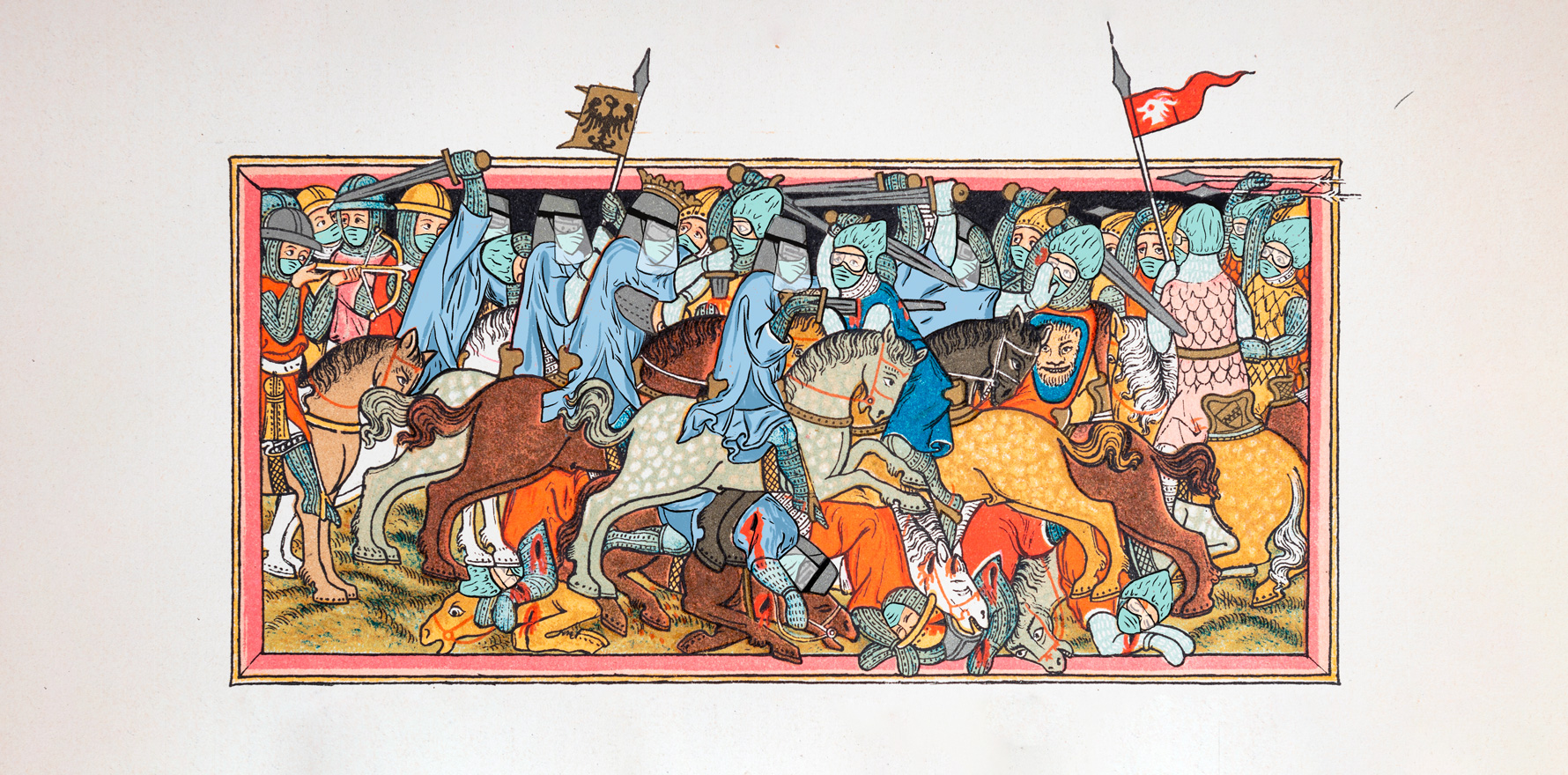
Adapted from the presentation “Healthcare is a battlefield” at DFTB22 Refresh with collaborator Dr Melanie Rule